Improve customer service with a comprehensive claims management system


While the Customer Portal allows the client to initiate claims, follow up on their processes, and provide additional information, the Back-Office guides the user through the entire process from an initial review to final settlement

Healthcare
- Medical malpractice claims
- Medical billing
- Insurance reimbursements
- Workers' compensation claims
- Patient injury claims

Insurance
- Auto insurance claims
- Property insurance claims
- Life insurance claims
- Liability insurance claims

Retail & Logistics
- Production liability claims
- Warranty claims
- Accident claims
- Consumer complaints
- Return and refund claims
Want to see how Junica's Claim Management can benefit your company?
Watch demo
Manage the full claim management lifecycle
Core capabilities
How does it work?
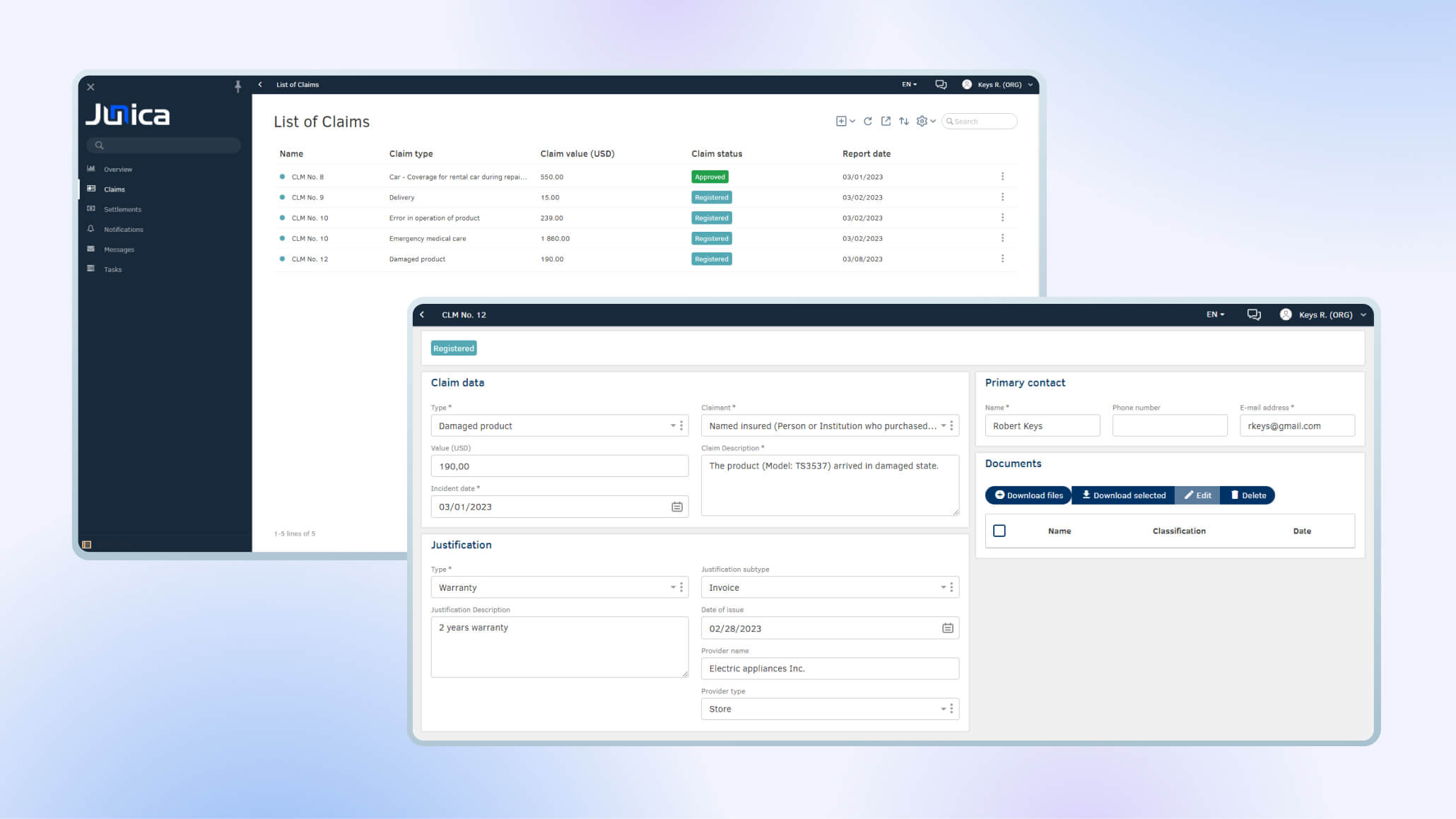
Customer Portal
Empower customers by providing a user-friendly platform to manage their claims effectively
After adding the necessary information, clients can submit their claims which means the request is sent to the back-office application via integration.
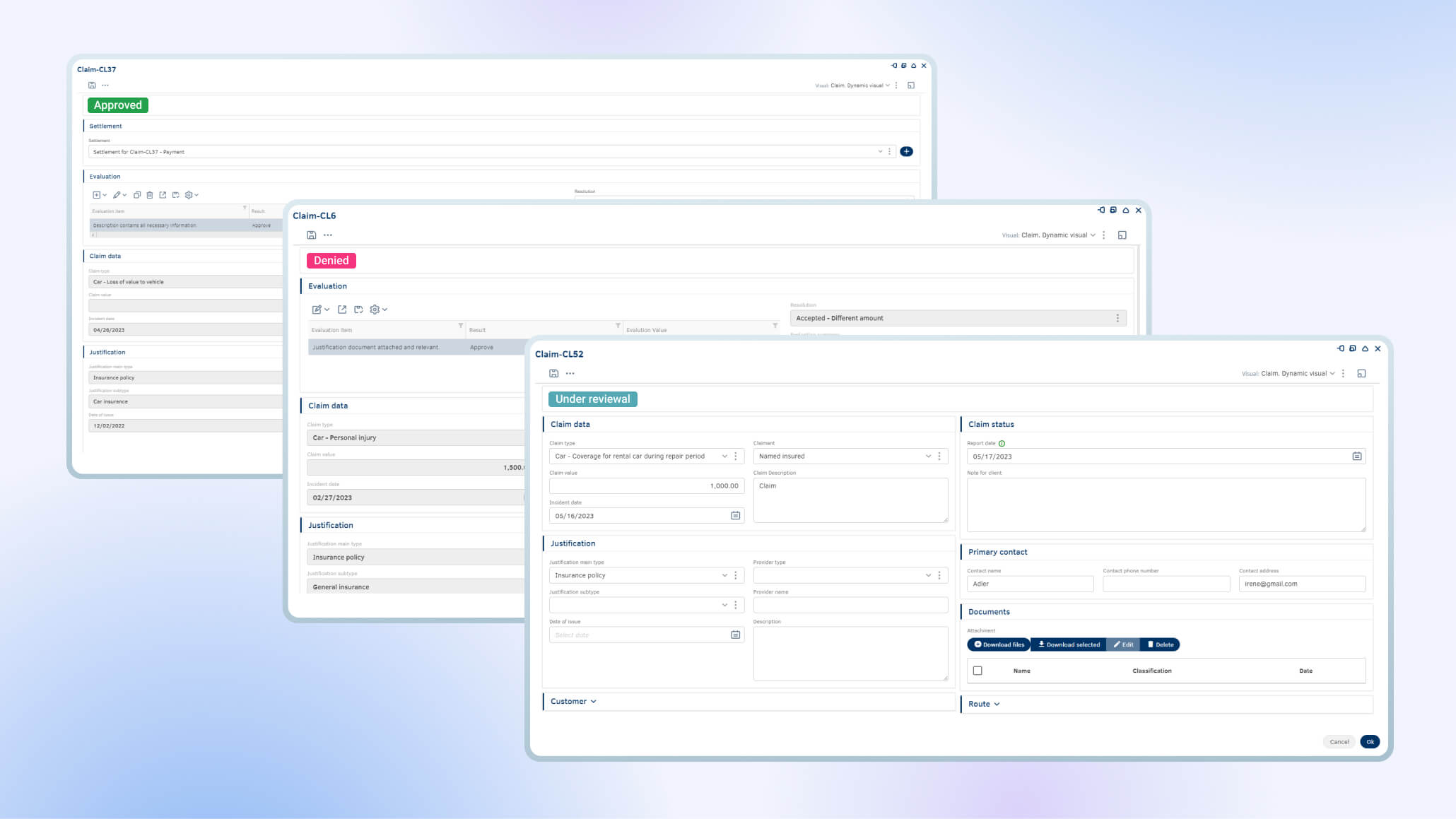
The settlement, which is the initial agreement with the claimant and parties involved, must be adjusted once each type of claim is evaluated: considering the case, insurance policy, and information relevant to the claim. Depending on the nature of the claim, the insurance type, and the industry, the settlement can vary and be tailored. In essence, the settlement establishes the type of compensation (reimbursement, reinstatement, replacement, repair) as well as the settlement agreement with the parties: the insurance provider, or the policyholder, details from vendors, etc.
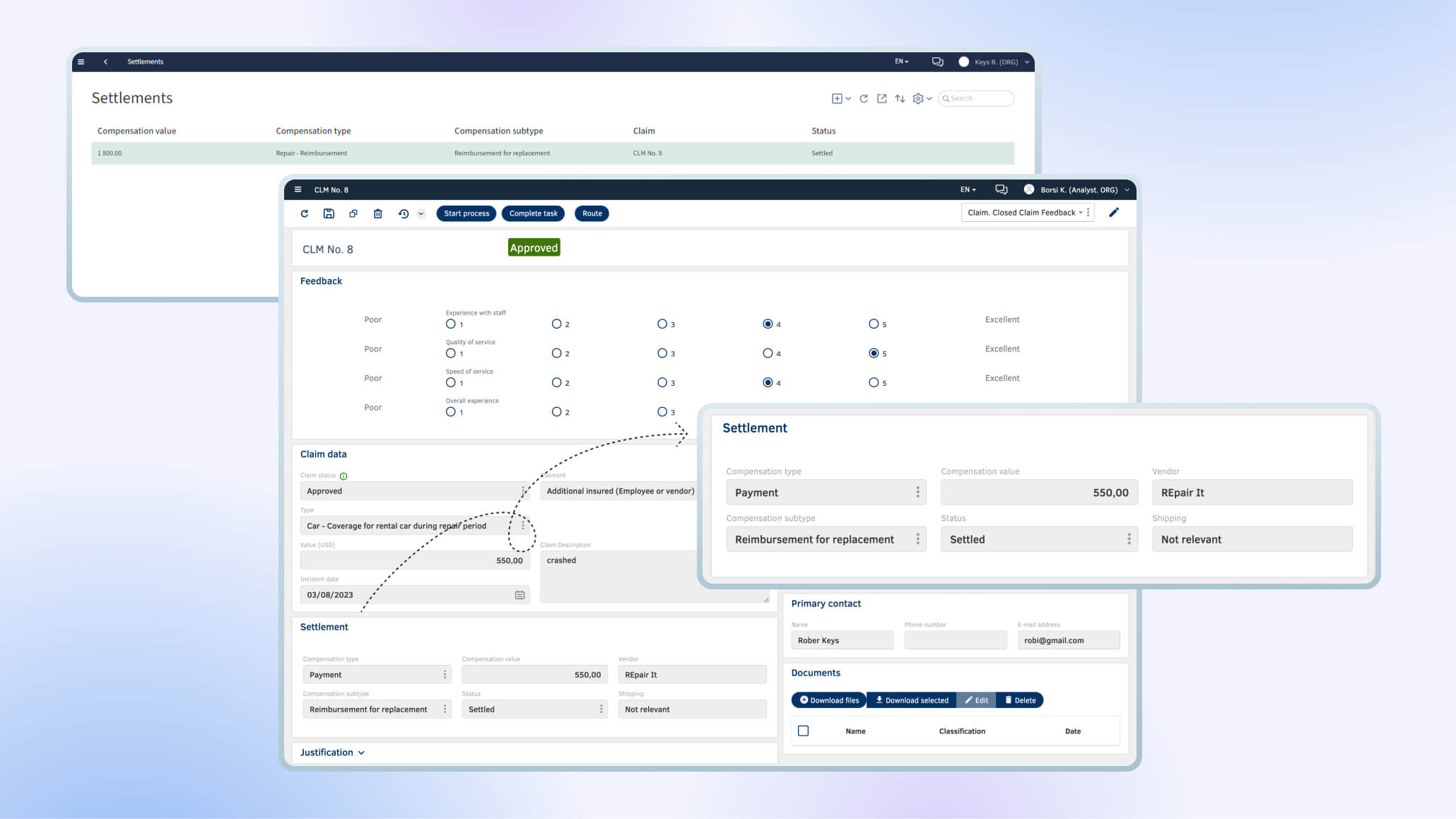
The final resolution establishes the final agreement, adjudication, status of the claim (favorable or unfavorable to the client) and the details relevant to the case: evaluation, documents, dates, justification, contracts.
How does it work?
Back-Office
Optimize claim handling, streamline processes, and provide efficient tools for management
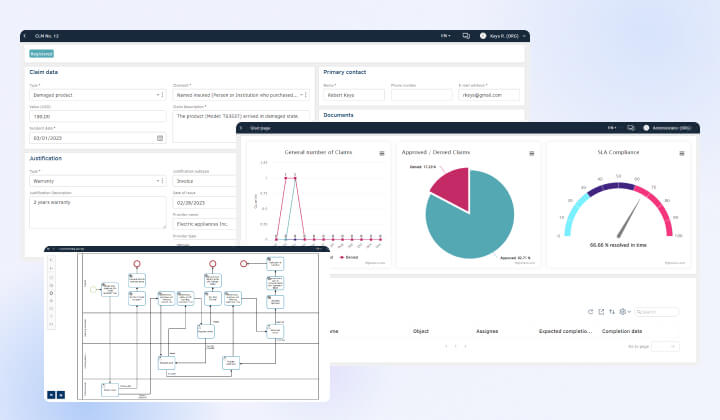
An analyst has an option to either send a claim to evaluation to the handling department or ask for some adjustments from the client. If the claim was sent to evaluation the handling analyst can add multiple evaluation items and a resolution. The customer will get the notification about the update with the summary.
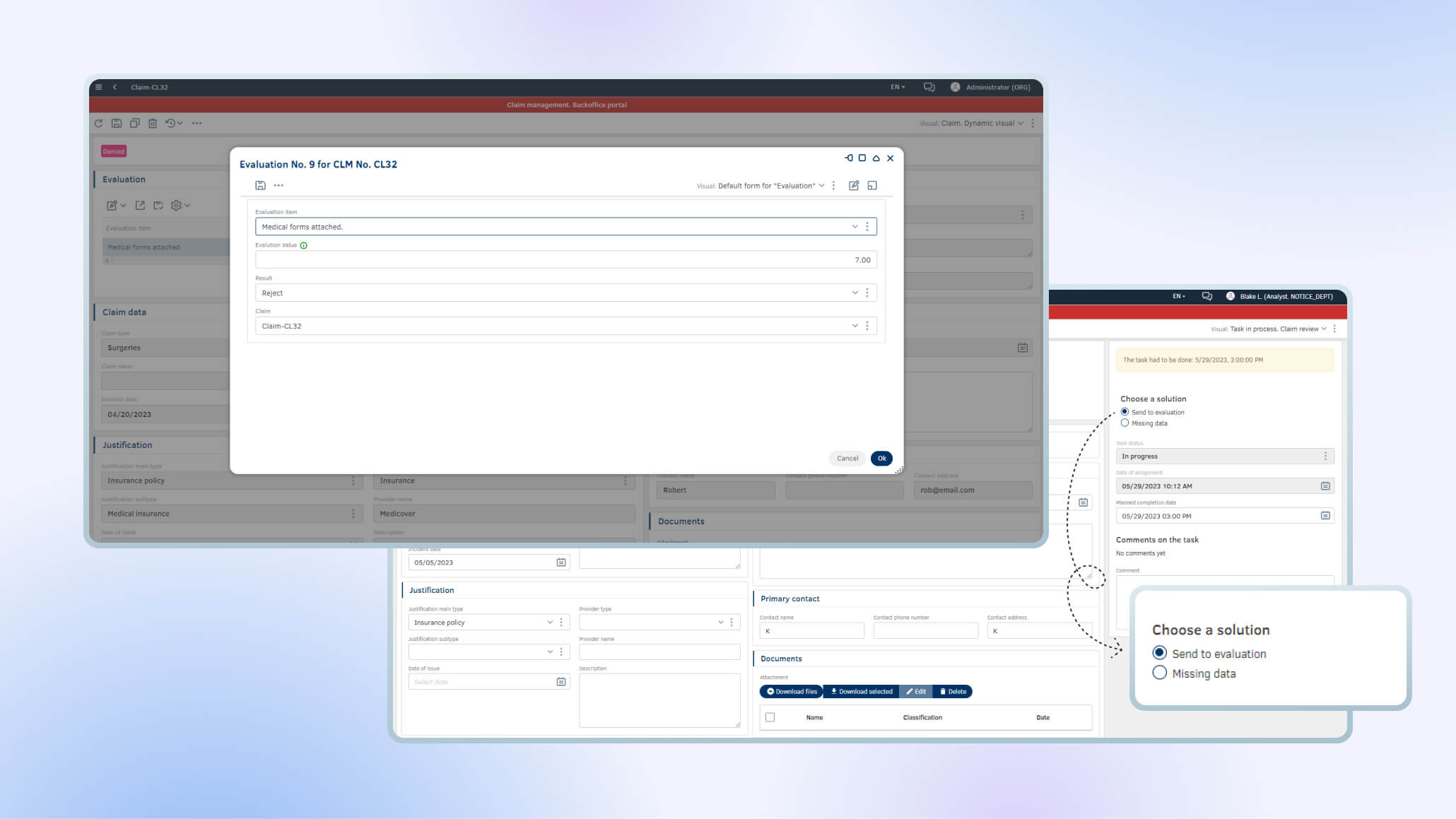
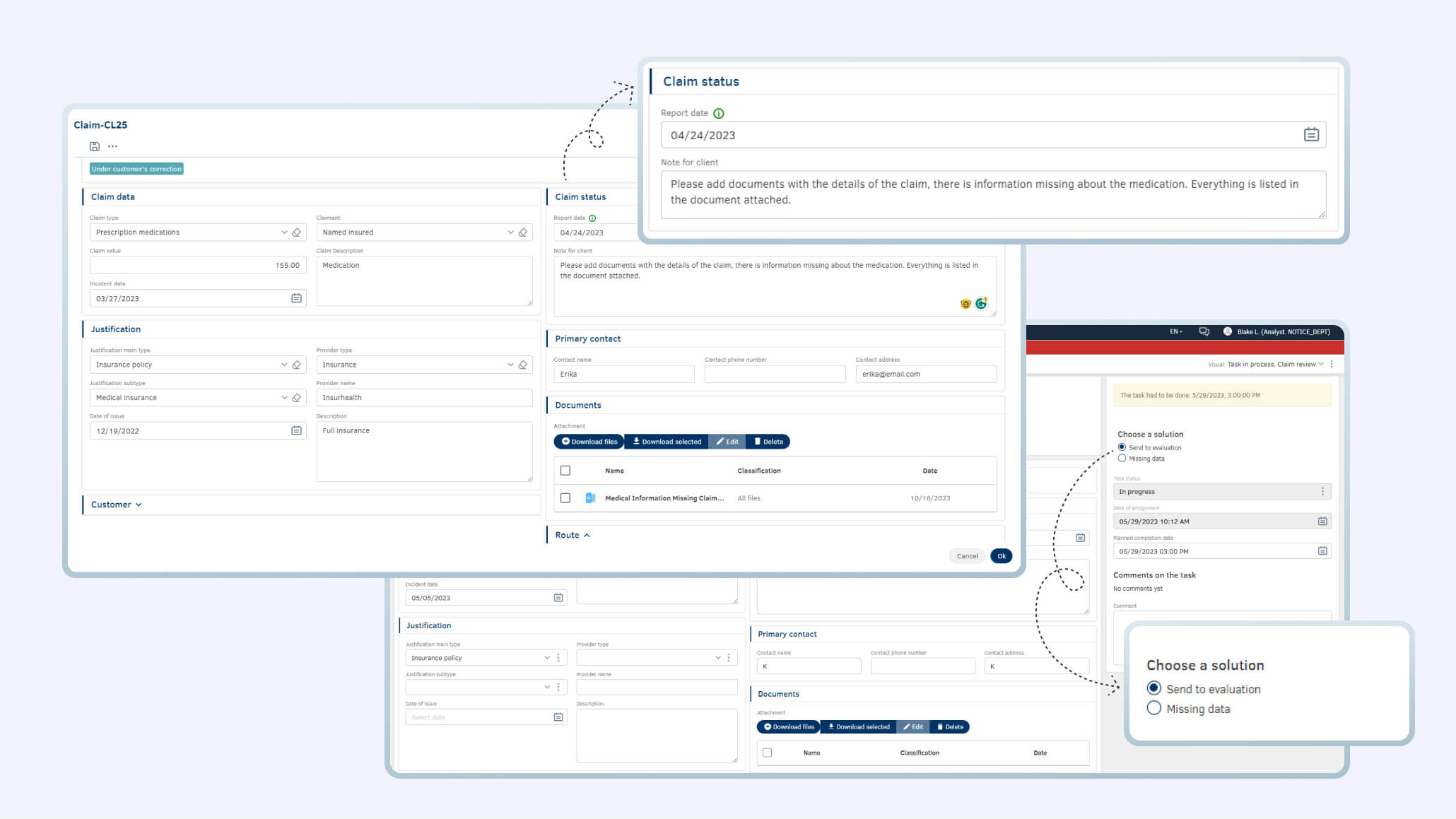
On Back-Office side the business process is designed to cover multiple scenarios such as requesting missing information from clients, necessary approvals and internal corrections of evaluation. The customer gets a notification about what they need to adjust in their application.
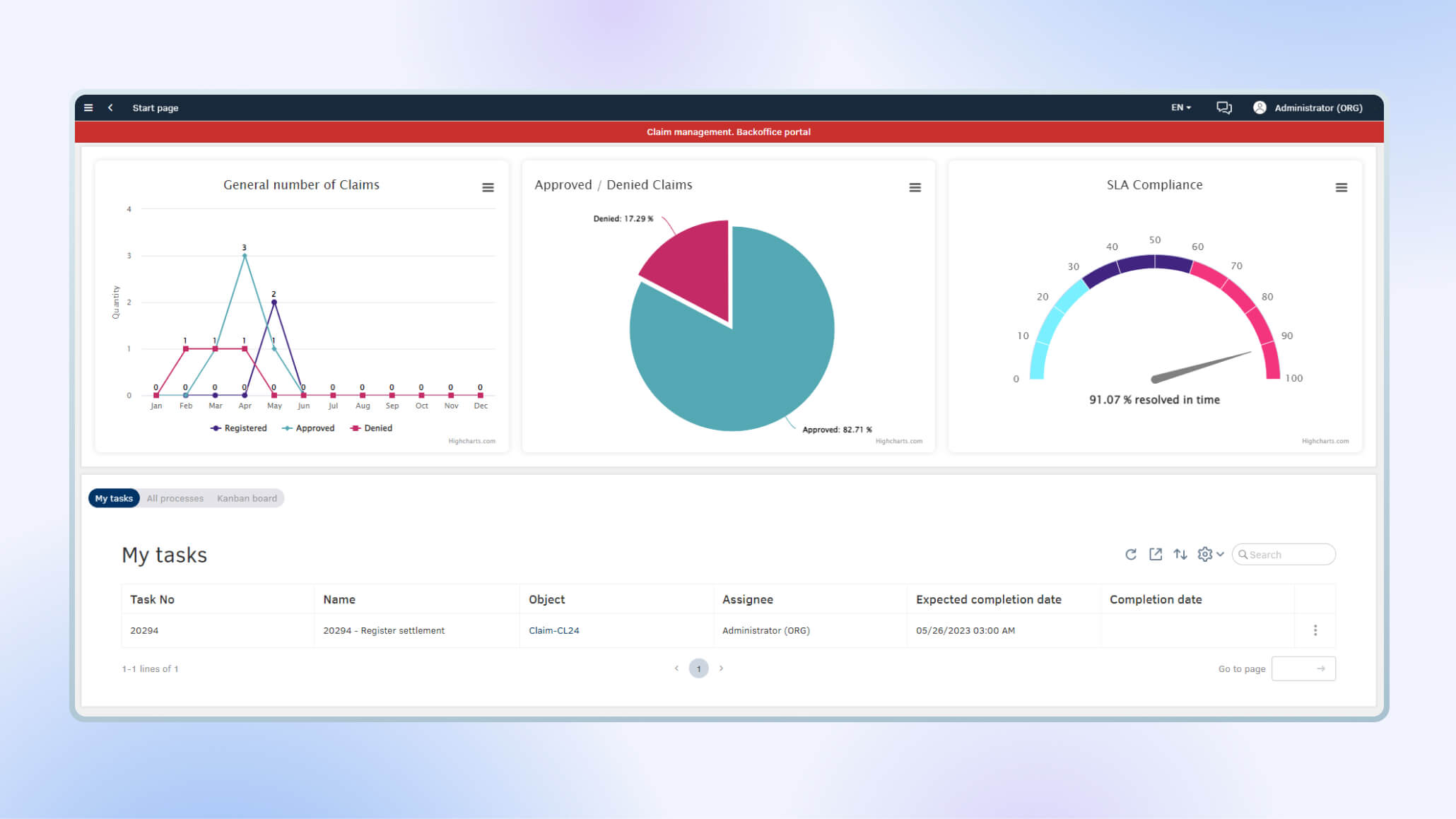
The analytics and reporting section display common and custom statistics of claims, it's volume, claim trends, filter by claim statuses, resolution time and also allows decisions makers to customize reports with information of their interest.
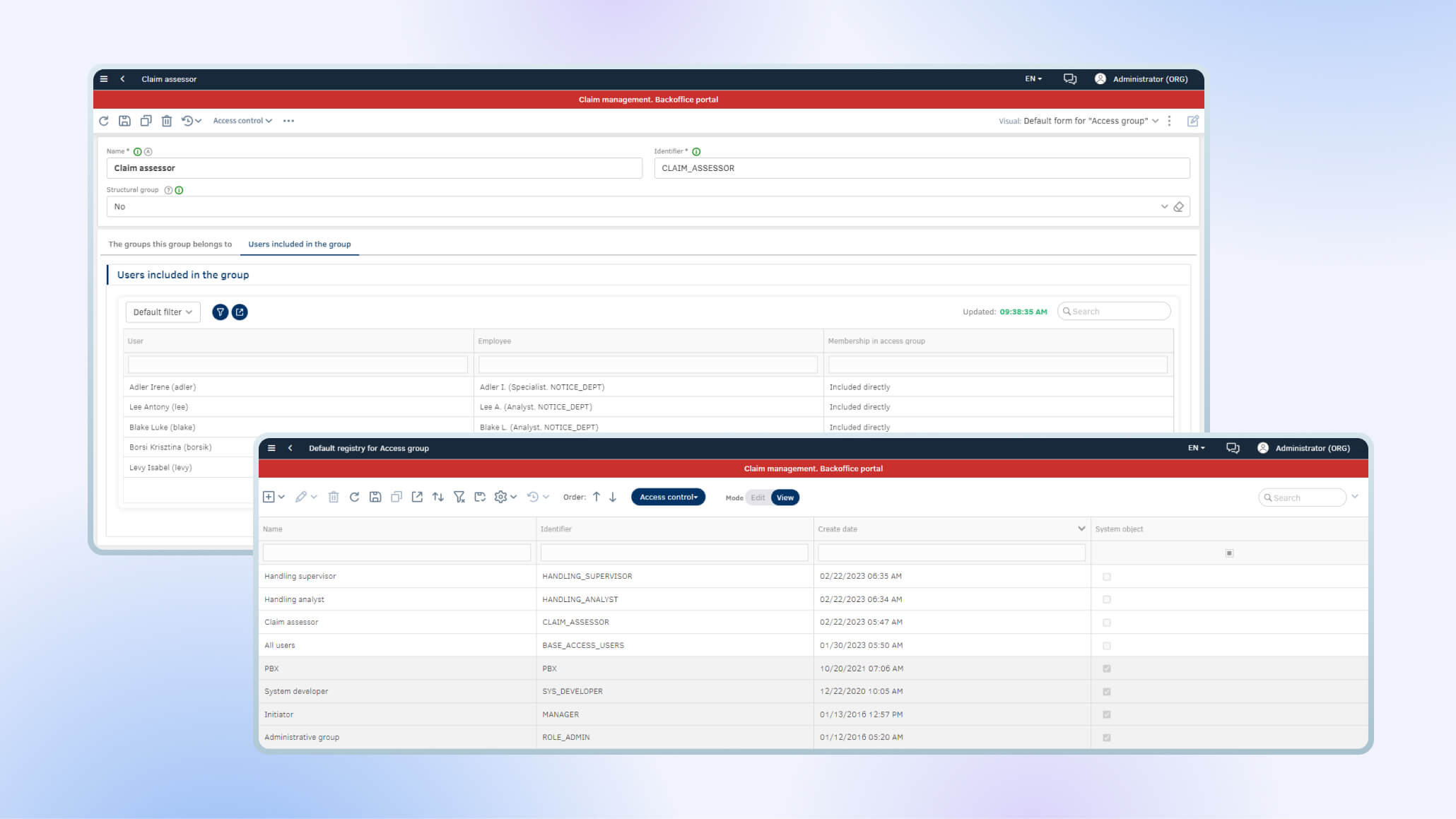
The Back-Office employees are divided into two main departments: Notice department, which is responsible for the initial review of new requests and Handling department which evaluates the claims and defining the proper settlements for each case. The platform allows the administrator to assign specific access rights to different user groups or users. The setup is under Administration, access control.
Connect to any data source
Thanks to the open API, the platform allows data exchange with all data sources: file systems, databases, web services, and message brokers.
Choose a robust claim management solution
Flexible
Low-code technology makes it possible to tailor your solution to your needs without programming
Scalable
The platform can be used by teams of any size and withstands high loads
Powerful
The solution implements cutting-edge low-code technologies with machine learning for complex calculations







